Kidney stone formation encompasses a series of common pathological disorders involving the formation of stone deposits within the kidneys. Several risk factors contribute to stone formation and progression, including genetic changes, biochemical/metabolic disorders, abnormalities in renal anatomy, and environmental factors, but determining why these factors contribute to stone formation is difficult and complicates the process. factors have prompted efforts to evaluate the mechanisms of intracellular stone formation through a simple model system, cultured renal epithelial cells, with a focus on the cellular response to oxalate, the most common mode of stone disease.
Whether oxalate is in a crystalline state or in a dissolved state, it can trigger cellular reactions within a certain range, which is beneficial to the formation of stones. This includes changing the properties of cell membranes, thus promoting stone adhesion, altering cell activity and providing fragments that facilitate nucleation of crystals. The activity of PLA2 in the cytosol plays an important role in the formation of oxalic acid, triggering the transmission of signals and producing several lipid regulators (arachidonic acid, amino acids, lecithin, Lyso-PC, ceramide), which Regulators act on important targets within the cell (mitochondria, nucleus), with the net effect of increasing the number of reactive oxygen molecules (which in turn can affect other intracellular processes), increasing cell death, and inducing continued growth in viable cells. Certain genes, some of which can promote cell proliferation to replace dead cells, or promote the secretion of macromolecular substances in the urinary tract, can regulate the formation of crystals.
1. Redistribution of membrane phospholipids
The early cellular response to oxalic acid is that phospholipid-phosphatidylserine (PS) is redistributed on the cell surface, instructing macrophages to phagocytose damaged cells, and the redistribution points of PS on the cell surface become calcium oxalate adhesion point. Because phospholipids are normally confined to leaflets within the cell membrane through activation processes involving the actin cytoskeleton, the redistributed state of PS on the cell surface can also induce the activation of enzymes associated with membrane junctions, including those leading to phospholipases. activation.
2. Lipid signaling molecules
In studies on oxalate activity in kidney cells, phospholipase A2 (CPLA2) has received the most attention. CPLA2 is an enzyme that hydrolyzes the acyl group at the Sn-2 position of phospholipids. After CPLA2 acts, it can produce some active substances, including arachidonic acid and lysophospholipids, which in turn can stimulate other information channels in cells. , this enzyme is also involved in the pathological process of renal epithelial cell injury. In fact, the arachidonic acid in the blood of patients with stones is increased, and the arachidonic acid on the red blood cell membrane is also increased. Interestingly, CPLA2 activity can determine the time-concentration relationship of oxalate in cultured renal epithelial cells. The two products AA and lysophospholipid after the action of CPLA2 can regulate the activity of oxalic acid, causing changes in mitochondrial function and gene changes. Oxalic acid can induce the activity of CPLA2 and has a certain effect on the production of ceramide. Signaling molecules are involved in a variety of cell injuries, from cell proliferation and differentiation to cell toxicity and death. All three lipid signaling molecules regulate oxalic acid. Role in salt-induced renal cell damage.
3. Oxidative stress
Early animal experiments and cell cultures showed that oxalate increases renal oxidation. Animal experiments show that when the urinary oxalate load is increased, lipid peroxide secretion increases and renal antioxidant activity decreases. Kidney cell cultures have shown that exposure of cells to oxalate increases the production of free radical products and lipid peroxides. Oxalic acid-induced toxicity and free radical products can be reduced in vivo. Oxalic acid can also be reduced in vitro through anti-oxidation, correcting mitochondrial electron transport disorders, increasing the expression of BCL-2 through genetic manipulation, and regulating mitochondrial permeability through protein regulation. Induced toxicity and free radicals.
In mammalian cells, mitochondria are the main site of oxidation. Mitochondrial disorders can cause programmed cell apoptosis. Some studies have explored the role of mitochondria in oxalate activity. In kidney cell cultures, it can be found that oxalate causes functional changes in mitochondria, including membrane depolarization causing an increase in various cellular reactive oxidative species (ROS). Oxalate effects can be mimicked by arachidonic acid, Lyso-PC and ceramide, and inhibited by PLA2. Thus, the mitochondrial membrane appears to be an intracellular target for the regulation of oxalate activity. Further support for this is the possibility that exposure of isolated mitochondria to oxalate or lipid signaling molecules can increase ROS production and increase thiol production on mitochondria. Oxidation and peroxides of mitochondrial membranes.
4. The relationship between oxidative stress and renal cell damage and death
In addition to the observed increase in ROS production, oxalate affects mitochondria in cells, can significantly increase the permeability of mitochondrial membranes, and increase pro-apoptotic factors. One study found that oxalic acid increased apoptosis and necrosis of renal epithelial cells. Mitochondrial oxalate activity can also be secondary to PLA2 activity. Because this effect can be inhibited by PLA2 inhibitors and can be modeled by the lipid signal generated by PLA2, these data extend to earlier studies that oxalate can increase mitochondrial membrane permeability and further support mitochondrial ROS production. In oxalate-induced renal toxicityrole in �.
5. Moderate response to oxalate
In addition to toxic effects on the kidneys, oxalates can induce modest responses that may enhance the survival of residual renal epithelial cells. For example, oxalate-activated channels can lead to kidney cell proliferation (a process that replaces damaged/dead cells), can increase the expression of some genes involved in proliferation, increase DNA synthesis, and at least reduce oxalate concentrations (when cells When proliferation exceeds cell death), the number of renal epithelial cells increases.
Additionally, oxalate increases urinary expression of macrophages, cells that normally limit crystal formation. For example, oxalate can increase the expression of osteopontin both in vivo and in vitro. Osteopontin is a macromolecular substance in urine that can inhibit oxalate, crystal nucleation, growth, aggregation, and cell adhesion to calcium oxalate. Attached effect. Exposure to oxalate increases the expression of these proteins (as well as other macromolecules in the urine). Increased expression of these proteins may result in modest function and further limit crystal growth and precipitation. Functions of oxalate, such as toxic effects, can be modulated by PLA2 and subsequent ROS production.
6. The relationship between cell damage and toxicity and stone formation
Many evidence supports a relationship between kidney cell damage and crystal adhesion. Damage to the renal cell monolayer can provide binding points for crystal adhesion. These points are normally covered by tight epithelial cells. The binding points include more PS, hyaluronic acid, and sialic acid/matrix proteins. Once these crystals adhere, the crystals can serve as the core of new crystals, a process that facilitates stone formation. At the same time, crystals on the cell surface can be phagocytosed by renal cells. Once the crystals are engulfed, the crystals can reappear basolaterally under the action of lysosomes, thus providing a core for stone growth within the renal interstitial cells.
Fragments from damaged cells can promote the growth of stones, and the fragments provide a core for the uneven nucleation of crystals. Human kidney cells contain an organic nucleus whose composition is similar to that of a cell membrane, and fragments of the kidney cell membrane promote uneven nucleation of crystals in artificial urine. Oxalate can activate cell channels and promote the formation of stones. The focus of the changes it produces is the enhancement of the adhesion of crystals to kidney cells.
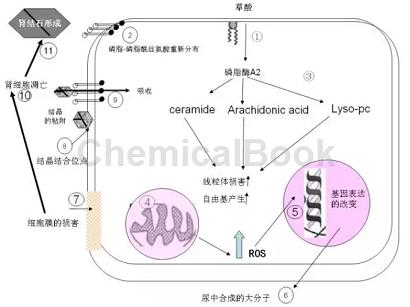
Picture of the effect of oxalate on the kidneys (Urol Clin N Am 34 xi)
(1) Oxalate can induce some changes in cell membranes.
(2) PS is redistributed and changes the membrane surface. Conducive to the combination of crystallization.
(3) Oxalate induces membrane dysfunction, which can lead to an increase in PLA2 activity, produce two lipid (arachidonic acid, LYSO-PC) signaling molecules and directly stimulate the production of ceramide.
(4) Lipid signals act on mitochondria, interfering with the structure of mitochondrial membranes, leading to mitochondrial dysfunction and increasing reactive oxidation products (ROS).
(5) Increase in ROS and/or LYSO-PC. Can change the expression of genes with certain functions.
(6) May also include proliferation (replacement of damaged cells) or secretion of urinary protein. (Formation of divided crystals).
(7) ROS also promotes cell damage.
(8) shows other crystallized binding sites.
(9) Adhering crystals can or become the nucleation core of new crystals. This facilitates stone formation.
(10) The endocytosis of crystals can aggravate cell damage. Endocytic crystals can be dissolved by lysosomes or appear on the basolateral side. Once again, it is the core of stone growth in renal interstitial cells.
(11) Oxalate causes cell death. Can produce cell fragments, which is conducive to the formation of other crystals and also promotes stone formation


 微信扫一扫打赏
微信扫一扫打赏
